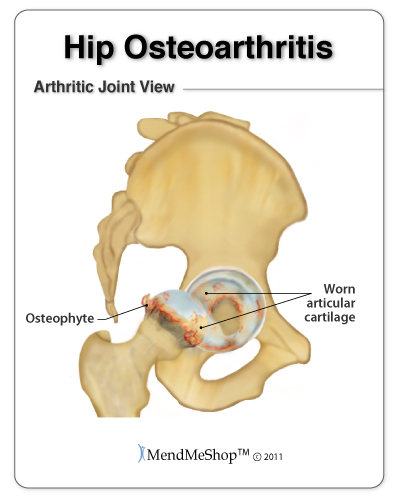
Arthritis in the hip is most commonly experienced as osteoarthritis, known as "wear and tear" arthritis. The hip, or acetabular joint, is a ball and socket joint which is lined with articular cartilage on the acetabular fossa (socket) and covers the head of the femur (ball). This fibrocartilage is a connective tissue that helps to hold the ball in the socket and provides cushioning so the bones do not rub against one another and can move smoothly in the joint.
Osteoarthritis affects approximately 12.1% of the United States population over the age of 25 (approximately 21 million adults). It is a progressive musculoskeletal, degenerative disease that wears away the articular cartilage and underlying bone in your joint(s), triggering chemical reactions within the joint that cause destruction. It can be very painful, it definitely weakens the joint and eventually becomes joint deforming.
Osteoarthritis occurs when this articular cartilage begins to degenerate. To put it more simply, the cartilage in your hip joint gets scraped and worn down. Over time, the head of the femur begins to rub against the acetabular fossa with little or no protection from the articular cartilage - as you can imagine, this increased friction causes a lot of pain. With this added friction, small bone fragments can break loose and float into the joint cavity, causing more aggravation. Space within the joint starts to decrease due to lack of cushioning, and stiffness in the hip becomes more and more of a problem. Eventually osteophytes, a protusion that develops from the joint cartilage, may form in the hip causing additional pain.
Swelling and excess fluid in the joint are common due to lack of natural protection that the fibrocartilage can no longer provide. This swelling and fluid further limit the hip's range of motion. The hip joint capsule and connected ligaments may then begin to thicken and shrink, and your leg muscles may weaken (atrophy).
Most sufferers report fluctuating symptoms that will worsen or improve over time. Factors that may affect the degree of symptoms of hip arthritis can include weather and/or your level of activity. Osteoarthritis usually develops slowly over the years. Unfortunately, there is no cure for arthritis or osteoarthritis but symptoms can be controlled, deterioration of cartilage can be slowed, and you can find relief from the pain.
The symptoms of hip osteoarthris can differ widely from person to person. This can range from very debilitating and occuring suddenly - to a mild development gradually over time. Sufferers may be experiencing few symptoms - even with obvious degeneration in their hip joint as shown on an X-ray. It is not unusual for someone with hip osteoarthritis to go pain-free for months or even years between episodes of greater pain symptoms.
Hip osteoarthritis symptoms don't generally affect other areas of your body. They are generally localized to one area; however they can affect people in different ways. Some people will only have a problem with 1 side of the hip, others will have it on both the right hip and left hip; some experience gradual pain with little change over the years, others experience vast changes in a short time period. Sometimes the cartilage on one side of the joint will wears out much faster than on the other side.
If you have hip osteoarthritis you may experience the following general conditions:
When you have early osteoarthritis in your hip you generally will experience the following symptoms:
Constant or Recurring Pain or Tenderness - Pain and tenderness in your hip joint can be ongoing and feel like a dull tooth ache pain, or it can be a sharp, throbbing pain with sudden movements. Typically, most hip osteoarthritis sufferes feel pain and tenderness in the groin, buttocks or thigh. If standing or walking, pain may be experienced on the side or back of the hip; the pain may also radiate down the thigh and/or even cause pain in the knee.
Pain is often worse in the morning or evening, or when you move your hip from a sitting to standing position (or vice versa), or when you participate in a prolonged walking or standing activity (non-movement). Changes in weather or different seasons of the year can make a difference to the sensitivity you feel in your osteoarthritic hip (however, hip pain can be experienced in all weather environments). As the atmospheric pressure falls/rises, the nerves in your hip are sensitive and react to pressure changes.
Stiffness will eventually be experienced in the affected hip joint, which will limit your range of motion so that you are not able to move your hips like you once did. This will make it difficult to climb stairs, or get in and out of chairs or bathtubs. This can result from periods of inactivity (morning stiffness, sitting, driving etc.), or after vigorous movement in athletic or work pursuits. Stiffness generally lasts up to 30 minutes however it can persist for longer periods of time. It will often be difficult to use or move your hip joint normally during this time.
Hip stiffness will result in your joint cavity producing extra fluid in the joint. This fluid, which is comprised of destructive proteins and enzymes, cause the cartilage and bones to deteriorate further and will cause swelling in the hip. The surrounding bone reacts by growing thicker. The bone at the edge of your hip joint eventually grows outward and develops into bony spurs (osteophytes).
Your hip joint tries to repair itself by creating osteophytes, however, they generally just make your hip more painful and difficult to move. Your joint capsule and ligaments slowly thicken and shrink, and your hip muscles weaken (atrophy), which in turn create instability in the hip joint (it gives way when you walk or put weight on it).
Swelling in your hip joint can occur immediately if your blood vessels are disrupted because of a traumatic event, or within 12 hours after your joint tissues become inflamed. Swelling over time is a result of synovial fluid filling the joint cavity, as your body tries to protect itself. Warmth and redness that sometimes accompany swelling are normally not associated with osteoarthritis.
As your hip osteoarthritis progresses, you may start to develop the following symptoms:
Deformity and joint enlargement will eventually result as your cartilage degenerates and bones become damaged. Bone spurs, cysts or overgrowths can develop as a result of ongoing hip symptoms due to your osteoarthritis. These are often tender when your skin is rubbed over them; and can result in irritation of other tissues and swelling. This can make it difficult to move your bones and can change the shape of your joint which force the bones out of their normal position and lead to deformity.
Grinding, Popping or Locking - Hip joint grinding, clicking, popping or locking when you try to bend or straighten your hip can result from arthritis, as well as other hip injuries. This can range from being annoying to downright painful and can last a few seconds or be persistent for a few weeks. Joint locking often occurs after long periods of inactivity, when loose fragments may become lodged in the joint. You will often feel a click or snap when it eventually unlocks. Sometimes you may have to manually move or manipulate your hip to get relief. You may experience your hip giving out because muscles in your hip, lower back, groin and thigh have weakened, or you have damaged ligaments and/or tendons in the hip joint.
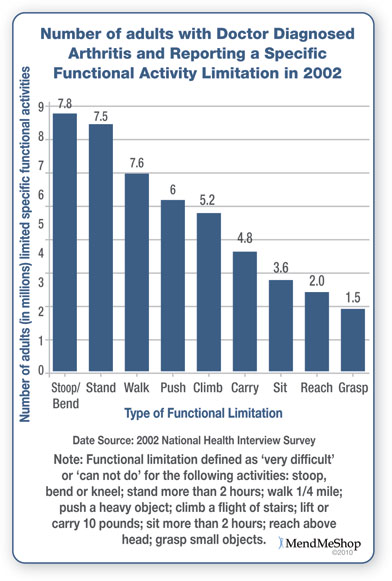
Difficulties Performing Activities - Functional limitation as a result of osteoarthritis is very common in daily activities, work and/or recreational pursuits. Osteoarthritis makes it very difficult to stoop, bend, kneel, stand more than 2 hours, walk 1 mile, push a heavy object, climb a flight of stairs, lift or carry 10 pounds, sit more than 2 hours, reach above your head and/or grasp small objects (as noted in the figure on the right).
Depression and Anxiety will often be experienced as the osteoarthritis symptoms progress and you start to feel like a hostage in your own body. These often leave you feeling fatigued, irritable, restless, hopeless, and guilty. Your pain and inability to participate in everyday activities may make it more difficult for you to concentrate and make decisions, and your interest in the people and things around may start to decrease. Overall your self-esteem and self-image really decline. However, it is possible to treat osteoarthritis symptoms, so you can start to feel more like your old self and begin to return to the activities you enjoy.
Unfortunately, there is no cure for osteoarthritis but symptoms can be controlled and, for most, you can find relief from the pain. Hip joint replacement, while being a major surgery, is found to be be worthwhile by an increasing percentage of osteoarthritis sufferers. Continual improvement and new techniques in joint replacement surgery are reflected in a steady increase in successful outcomes.
Arthritis is your hip's biggest enemy, and it can result over time from injury or disease. Osteoarthritis in the hip is common and there are a number of causes that influence your risk of developing it. These can be broken down into 2 types: primary osteoarthritis and secondary osteoarthritis.
This is a slow, progressive arthritis condition that usually begins after 40 years of age. It mainly affects weight-bearing joints (like knees and hips) as a result of excessive loads placed on normal joint tissues, or reasonable loads applied on inferior joint tissues. The exact cause is not determined however it is believed to be affected by:
This type of arthritis often appears before 40 years of age. It is the result of a clearly defined cause, such as:

The progression of osteoarthritis can be classified into 5 stages of severity:
As mentioned previously, the most common form of arthritis in the hip is osteoarthritis; however you can be diagnosed with more than 1 form of arthritis at a time. Medical professionals (such as an orthopedic surgeon or physician) will be able to assess and test whether you have arthritis, and then will determine what type you have through a variety of processes.
To help your doctor achieve a proper diagnosis, he/she will begin with a medical history about you, your current condition and symptoms. They will inquire about the intensity of your present pain, the duration of your symptoms and the limitations you are experiencing. Details about what instigated the problem, when it started, and whether or not you have ever had treatments for this or a similar condition in the past, are very helpful in assessing your injury.
A physical examination will be performed to determine if you have any signs of hip arthritis or other injuries pertaining to the lower back, hip and probably the knees. Your doctor will assess and palpate (feel) the bones and soft tissue in and around both hip joints to evaluate symmetry and recognize differences. This will identify any abnormalities, such as mild or severe inflammation, fluid, bone deformity, and weakened muscles. He/she will press on the injured side of your hip joint to test for point tenderness and help determine the main location of your injury. He/she may ask you to complete a series of knee and hip movements, or rotating your hip to see what motions cause pain, weakness, instability and/or grinding, catching, popping or locking. These sounds or restrictions will often indicate a soft tissue tear and/or arthritis in the knee or hip.
A medical professional will often recommend diagnostic testing to obtain more detailed information, and assess the amount and/or type of damage done to your hip. There are a variety of different tests available to help them analyze the situation; however these will be dependent on the degree of your injury.
X-rays provide a two-dimensional image of the overall structure of your hip. They are helpful in identifying loss of joint space, arthritis, abnormal bone shapes such as bone spurs or bone cysts, fractures, and degeneration (wear and tear) on the joint.
X-rays can also be helpful to exclude other possible causes of hip pain and assist the doctor in determining if surgery should be considered for your specific situation.
An MRI will provide more detailed information and will help to evaluate the state of soft tissue in and around your hip joint (muscles, tendons, ligaments, cartilage, other connective tissues).
It can identify ligament and tendon damage, and help to determine the extent of your injury, the displacement and degree of soft tissue tears, fluid in the hip, and/or other associated conditions.
Joint aspiration (arthrocentesis) involves withdrawing and analyzing fluid from your hip via needle and syringe. Arthrocentesis will help to determine (1) if there is inflammation and (2) the cause of your joint swelling - gout for example, or some kind of infection. Arthrocentesis can be performed in your doctor's office.
Blood tests cannot diagnose osteoarthritis, but may be ordered to rule our other causes of hip pain, like rheumtoid arthritis.
Arthroscopy is used to visualize and repair damage to the hip. A small incision is made in the hip and an arthroscope with a camera is inserted to look inside the the hip joint and assess any damage.
Further diagnostic tests such as CT or CAT scans (computerized tomography) or diagnostic ultrasound can be used to determine the degree and location of your injury if required.
The initial treatment for osteoarthritis is reducing the inflammation within the hip joint to relieve your pain. Anti-inflammatory medications can be helpful but be cautious of using them over a long period of time. These medications also affect the organs in your body and can lead to other problems with extended periods of use.
Once your medical professional has diagnosed your osteoarthritic condition, they will recommend the most effective treatment for your hip arthritis based on you and your lifestyle. They will consider your activity level, your age, the location and severity of your hip arthritis, as well as how long you have had it, the symptoms you experience and any other associated hip injuries. The treatment for a 34-year old athletic, working woman will not be the right treatment for a 75-year old retired man. Also, the treatment for a high energy, competitive or aggressive type-A personality, may not be suited to an easy going, relaxed and patient type-B personality.
There really isn't a cure for osteoarthritis. Generally, the focus of treatment is to relieve and control your hip pain and inflammation, slow down your arthritis progression, minimize your hip joint damage, maximize your hip mobility and function, improve your muscle strength and control, prevent work disability, and improve or maintain your quality of life.
Conservative treatments are usually recommended in the beginning. However, as your arthritis progresses, treatments that once worked may no longer be effective. Surgical options are used if conservative treatments fail, and your hip damage and pain severely interfere with your daily living. During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort in your hip area until your pain and inflammation settle.
The best way to manage your hip arthritis is to be one step ahead of the process, combining conventional practices and medicines with alternative treatments, joint protection, patient education, lifestyle changes if required, and self-management (diet, rest, exercise). The more diligent you are with your treatment and rehabilitation, the faster you will see successful results.
People with early osteoarthritis in the hip tend to have higher success rates than individuals with later onset, as their conditions are generally a result of trauma to healthy tissue rather than degeneration over the years. Scar tissue will often develop as a result of injuries once acute inflammation begins to decrease. As your damaged hip tissues heal this dead, fibrotic tissue will remain instead of forming brand new healthy tissue. Scar tissue adheres to muscle fibers, tendons, ligaments, fascia, nerves, and joints, causing pain and preventing them from moving properly (this limits your range of motion, flexibility and strength).
Reducing stress on the affected joint is a good idea, regardless of the choices you might make to manage your arthritis pain and inflammation. Losing excess weight and/or using a cane can take the pressure off the hip joint which will result in less irriation, inflammation and pain. Resting the hip as much as you can is also recommended to prevent further irritation in the joint.
Although, there really isn't a cure for osteoarthritis you can minimize the symptoms so it is less disruptive in your everyday life. Generally the focus of treatment is to:
When a tear first occurs or when it is irritated by overuse or re-injury, you experience swelling and inflammation in your hip. Using ice packs to treat your hip reduces pain, swelling, and tissue damage.
Ice packs work by slowing nerve and tissue function in the hip. This is important because once blood vessels are damaged, they can no longer carry oxygenated blood to soft tissue. As this occurs, cells begin to break-down.
Once inflammation and swelling have been reduced in your hip, nourishing and strengthening the tissue in your joint is the goal. Circulation Boost promotes blood flow to the treatment area bringing the necessary oxygen and nutrients to your weakened soft tissue. This increase in blood flow should, in most cases, maximize the ability of the body's natural soft tissue repair process.
Increased blood flow helps whisks away dead tissue and toxins (including lactic acid, commonly found in trigger points) that have built up from the injury leaving the area clean and better prepared for healing. Our Back/Hip TShellz Wrap® provides effective, non-invasive, non-addictive pain relief with no side effects.
Keeping your hips as healthy and strong as possible throughout the healing process will allow you to get back to your regular activities faster. The benefits of Circulatory Boost do not end once your hip pain stops. A TShellz Wrap® treatment before activity is an easy way to warm up the soft tissues in the hip to prepare them for use (so they are more flexible and less likely to strain when stretched during activity). End your day with another treatment to prevent tightness from setting in overnight.
During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort in your hip area until your pain and inflammation settle. With these conservative treatment protocols you should notice great improvement within a few weeks, with most meniscus patients seeing some improvement quickly. The more diligent you are with your treatment and rehabilitation, the faster you will see successful results. If you start using your hip before it has a chance to heal properly (even though it may feel better), you can end up doing a lot more damage than good!
Resting the area of injury, for our natural process to heal the tissue needs time. Not resting an injury can bring about the issue of an injury not going away (chronic). To repair damaged tissue, the bodies quickest way to heal is to create scar tissue and adhesions - this is good in the short term, but in the long term will be problematic.
The growth of scar tissue and adhesions can lie in any direction. Ultimately what causes stiffening in the tendon and muscle, entrapping a nerve, restricting movement, less elasticity, poor circulation, and flexibility.
Unfortunately, scar tissue may plague you for weeks, months and maybe even years, depending on your level of activity and the amount of conservative treatments you have done during your rehabilitation. Scar tissue is a major problem, especially when it comes to re-injury of your tendon or muscles. When dealing with scar tissue it is always important to:
Continue the healing process by resting your joint. Limit your movements that may aggravate your strain as this might lead to re-injury. Tendon / Muscle related injuries can easily turn from a grade 1 strain into a grade 2 or a grade 2 into a grade 3 injury.
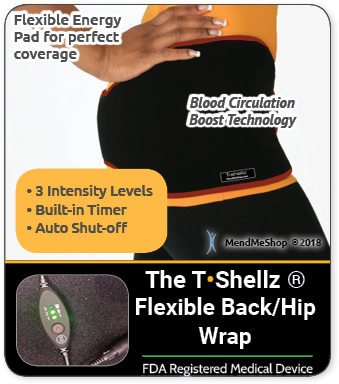
Whether you want to reduce your risk of further damage to your soft tissue injury, avoid re-injury, or manage pain and increase circulation for lifelong health benefits, we feel that TShellz Wrap® can provide exceptional results. Why spend time in pain, off from work, and missing out on your active lifestyle when you can be proactive about your injury and the health of your body? Talk to your doctor about incorporating a regular routine of using a Cold Compress or Ice Pack and a Back/Hip TShellz Wrap® into your everyday health regimen.
Product Advisors are available 9:00 am to 5:00 pm Eastern Standard Time Monday to Friday.
I want to learn more about Hip Surgery & Post-Surgery Recovery
I want to learn more about Circulation Boost
I want to learn more about Ice & Heat: Which Is Better For The Hip?
I want to learn more about Trigger Points in the Hip
I want to learn more about Hip Surgery: Do I Need It?
During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort at the location of your soft tissue injury until the pain and inflammation settle. The more diligent you are with your treatment and rehabilitation, the faster you will see successful results!
Please be aware that this information is neither intended nor implied to be a substitute for professional medical advice. CALL YOUR HEALTHCARE PROVIDER IMMEDIATELY IF YOU THINK YOU MAY HAVE A MEDICAL EMERGENCY. Always seek the advice of your physician or other qualified health provider before using any of our outstanding products to make sure they are right for you and your condition or if you have any questions regarding a medical condition. Always see your doctor for a proper diagnosis as there are often many injuries and conditions (some very serious) that could be the cause of your pain.
© 2025 In.Genu Design Group, Inc. Contact Us